Erin Green DDS
Sponsored By Ivoclar
Treating patients with TMD disorder caused by chronic grinding or clenching can be a challenging and often long process that can take months or even years to correct. Patients often present with severely worn dentition resulting in severe tooth sensitivity. As CEREC® dentists, we are accustomed to and pride ourselves on the ability to provide same-day dentistry. Even when we have a case that requires more than one visit, the case is usually resolved within a couple of days or a week. Occasionally, however, we are presented with a case, such as the one reported here, that requires multiple phases of treatment, with each phase carefully evaluated to ensure a decrease in TMD symptoms and a resolution of tooth sensitivity.
Case Report
The patient is a 45-year-old female with a history of chronic jaw pain and complaining of severe tooth sensitivity. She also was unhappy with the appearance of her worn dentition and very self-conscious of her smile (Figure 1). Past dental treatment to alleviate these issues included multiple nightguard/TMJ splints, therapeutic Botox treatment to relieve jaw pain, topical treatments for tooth sensitivity, and regular use of prescription strength fluoride toothpaste.

Figure 1: Patient presented to the practice unhappy with her smile and complaining of a history of jaw pain, worn dentition and severe tooth sensitivity. A full mouth rehabilitation was proposed.
After a complete exam, the treatment plan proposed to the patient was a full mouth rehabilitation to restore lost tooth structure and missing teeth and improve the position of her jaw. The first phase of treatment would involve restoring the upper arch to address the patient's primary complaint of an unattractive smile and placing implants in both arches to address lost or missing tooth structure.
Although endentulous site #30 was determined suitable for implant placement, upon closer examination edentulous site #14 was deemed unfavorable due to a lack of restorative space, and it was recommended the site be restored with a 4-unit bridge. Vertical dimension of occlusion would need to be opened 1mm with crowns on upper and lower posterior teeth to ensure optimal esthetic proportions for maxillary and mandibular anterior restorations. Each phase of treatment would require the fabrication of new upper and lower nightguards to prevent grinding and damage to restored teeth.
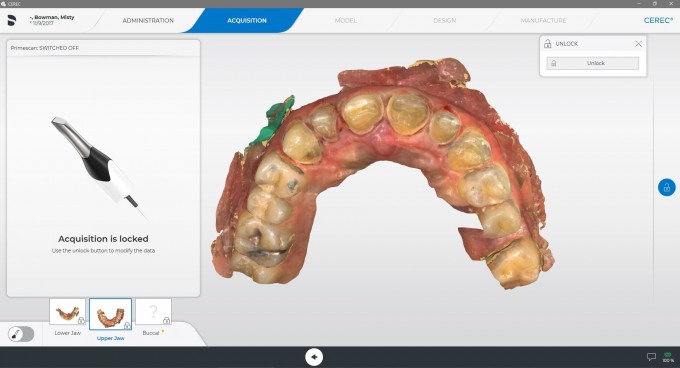
This four-year treatment process began in July of 2017 with placement of an implant at tooth site #30 and restoration of her upper arch. To gain enough vertical dimension of occlusion to ensure esthetic proportions for the anterior crowns, teeth #4 and #5 were prepped for single crowns and teeth #12-#15 for a bridge. The preparations were scanned and imported to CAD software for design and milling of the full contour crowns (Figures 2 and 3) and 4-unit bridge (IPS e.max CAD, Ivoclar Vivadent). Once the patient approved the new bite, restoration of her worn anterior teeth #6-#11 could be executed. The teeth were prepped, scanned and full-contour crowns CAD designed, milled and seated (Figures 4 and 5) (IPS e.max CAD).


Figures 2 and 3: To gain enough vertical dimension of occlusion to ensure esthetic proportions for anterior crowns, teeth #4 and #5 were restored with single crowns and a 4-unit bridge on teeth #12-#15.

Figures 4 and 5: Vertical dimension was achieved to ensure esthetic proportions for crowns on teeth #6-#11.
However, at a later appointment, the patient complained she could not tolerate the 4-unit bridge on teeth #12-#15 and opted instead to restore those teeth with single crowns on teeth #12, 13, and 15 (Figure 6). The single crowns were milled and seated, and implant site #30 restored with a full contour crown, completing the upper arch restoration.

Figure 6: The 4-unit bridge placed on teeth #12-#15 was replaced with milled single full contour crowns after the patient complained she had difficulty tolerating the bridge.
Over the next couple of years, the patient reported that symptoms of her TMD had remained unchanged and in March of 2021 was ready to initiate treatment of her lower arch.
A Lucia jig was used to capture and restore the patient's centric relation. Her VOD was increased by 1mm. Teeth #18-#21 and #29-#31 were prepped and overlay restorations designed (Figure 7), fabricated (Tetric CAD, Ivoclar Vivadent) and seated.
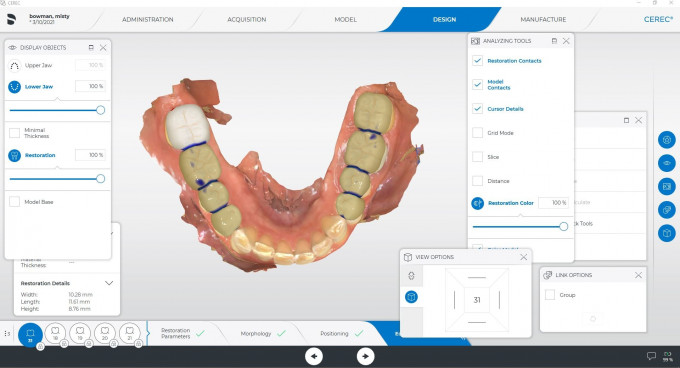
Figure 7: Onlays were designed and seated on teeth #18-#21and #29-#31.
In June of 2021, the patient reported she had adjusted well to the new bite, which had decreased her TMD symptoms and lessened her desire to clench and grind her teeth. At that appointment permanent restorations for her lower anterior teeth were initiated. For severely worn lower anterior teeth #22-#27 (Figure 8) veneers were prescribed. The teeth were prepped (Figure 9) and veneers designed, milled and seated. The full arch rehabilitation was completed with replacement of the Tetric CAD overlays on teeth #17-#20 and #29-31. IPS e.max CAD veneers were milled and seated at the approved centric bite position (Figure 10). All restorations were milled of IPS e.max CAD MT shade B1 and cemented with Adhese Vivapen/ Variolink Esthetic combo (Figures 11-14).

Figure 8: To restore the patient’s worn lower dentition, veneers were prescribed for teeth #22-#27.

Figure 9: Final veneers were seated on teeth #22-#27.

Figure 10: The Tetric CAD onlays were replaced with IPS e.max CAD veneers on teeth #17-#20 and #29-#31, completing the restoration of the lower arch.


Figures 11-14: The full mouth rehabilitation restored the patient’s smile, resolved her tooth sensitivity issue, and continues to decrease her symptoms of TMD.
The patient was thrilled with her new smile and continues to report decreased TMD symptoms and complete resolution of tooth sensitivity.


 Erin Green
Erin Green